The Neuroscience of Stress: Understanding What Causes Stress in the Brain
In the modern world, the problem of mental and somatic disorders associated with stress is becoming increasingly important. On the one hand, stress is the most important evolutionary mechanism necessary for the body to adapt to changing environmental conditions. On the other hand, long-term exposure to stress factors can lead to depletion of the body’s physical resources and the development of comorbid (associated) disorders.
First of all, this is due to the launch of protective and adaptive reactions at the cellular, physiological, and behavioral levels. The perception of stress stimuli and, as a result, adaptation is based on a multi-stage interaction of the structures of the central nervous system (CNS) and peripheral organ systems, including the immune system. The main “link” of this interaction is special cells of immune origin–microglia.
Depending on the environmental conditions and the nature of the stress effect, microglia cells can acquire various morphofunctional phenotypes, demonstrating amazing “flexibility” of the adaptive response. In the article, we will discuss what mechanisms are responsible for the brain’s adaptation to stress at both the cellular and systemic levels.

How Does The Brain Perceive Stress?
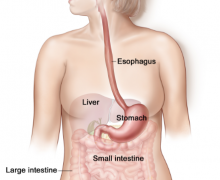
Firstly, let’s look at what part of the brain controls stress. In the brain, the structures of the limbic system (amygdala, prefrontal cortex, hippocampus and hypothalamus) associated with higher cognitive functions, such as emotional memory and fear-conditioned learning, participate in the perception of stress stimuli. They transmit a signal of danger to the main center of vegetative and endocrine regulation and homeostasis control – the hypothalamus.
An increase in the level of hypothalamic hormones–vasopressin and corticotropin-releasing hormone (corticoliberin)–leads to activation of the hypothalamic-pituitary-adrenal axis and an increase in the synthesis of adrenocorticotropic hormones of the pituitary gland and glucocorticoid hormones of the adrenal cortex (mainly cortisol in humans and corticosterone in rodents).
Understanding how your own stress response might be shaped by early experiences can be a powerful first step toward better mental health, take the ACE test (Adverse Childhood Experiences (ACE) to gain insights into your personal stress risk factors.
Finally, the release of catecholamines (adrenaline, noradrenaline, dopamine) into the bloodstream has an activating effect on the body and triggers the so-called “fight or flight” response. It consists of mobilizing the body’s energy resources in response to a threatening stimulus: glucose and fat metabolism are activated, and their delivery to the muscles increases, as well as the respiratory rate and heart rate increase.
However, another mechanism plays a major role in the pathogenesis of stress-associated diseases–hyperactivation of the immune system and an increase in the level of hormones and inflammatory mediators, which lead to the development of systemic and neuroinflammation.
The Role of Inflammation in the Development of Stress-Associated Disorders
The role of neuroinflammation in the pathogenesis of stress-related diseases is indicated by the results of numerous studies. For example, an increase in the level of proinflammatory cytokines in the peripheral blood and central nervous system was found in patients with depression, as well as in animals in experimental models of depressive disorder and chronic stress. Thus, long-term stress becomes an independent risk factor for the development of concomitant mental and somato-vegetative disorders.
Stress and the Brain: Adaptation Possibilities
“Communication” between the brain and the immune system is provided by the only cells of myeloid origin in the central nervous system – microglia, which account for 5% to 20% of all glial cells. Microglia cells are formed from primitive macrophages of the yolk sac and enter the brain at an early stage of embryonic development.
In the postnatal period, microglia participate in the regulation of the formation of dendritic spines and synaptic plasticity, and in the adult brain, they ensure the maintenance of homeostasis of the microenvironment, memory processes, synaptic plasticity, and neurogenesis. In case of brain injury, microglia also perform a number of protective functions.
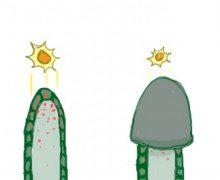
Depending on physiological conditions, microglia can acquire various morphological and functional characteristics (phenotypes): in a resting state, the cells have a branched morphology with short and thin processes (resting form), and under adverse conditions, they acquire an amoeboid or reactive form.
The Effect of Stress on Microglia: Experimental Research Data
Researchers from Fudan University in China studied the effect of stress on microglia. The scientists used an experimental model of mild, unpredictable chronic stress, which is as close as possible to real conditions: it allows them to “reconstruct” the effect of regular moderate stress, such as social stress, on humans.
The stressors used were being in a cramped cage (crowding effect), immobilization (restricted movement), mild cold exposure, frequent changes in light conditions, etc. The authors of the study assessed the anxious and depressive behavior of mice, as well as morphological changes in microglia cells (in almost all areas of the brain, except for the olfactory bulb and cerebellum) after 12 weeks of daily stress exposure. The experiment was conducted on males due to their more “pronounced” microglia cellular phenotypes.
Results of the Study
Exposure to chronic stress for 12 weeks led to changes in the morphology of microglia cells, increasing the number and length of their processes. Scientists found similar changes in other structures of the limbic system – the dentate gyrus, hippocampus, and amygdala. In the subpopulation of “interferon microglia” cells (one of six subpopulations of microglia), transcription of interferon-regulated genes (IFG), involved in immune cascades, was reduced.
At the same time, the expression of the interferons themselves remained at the same level. Thus, although long-term stress did not affect the synthesis of interferon IFN-β itself, it led to a decrease in the expression of genes for other interferons, including proinflammatory type I interferons and links of the IFN-γ-mediated signaling cascade (anti-inflammatory type II interferons).
IFN-β is a cytokine that is released by innate immune cells and some non-immune cells. It can have both anti-inflammatory and pro-inflammatory effects and is involved in the regulation of virtually all links of the innate and adaptive immune response.
While abnormally high interferon production causes a disruption in the regulation of the corresponding signaling mechanisms, the absence of changes in their levels in the brain and spleen against the background of a decrease in the expression of IFN-regulated genes may indicate the presence of another microglia phenotype. This phenotype is formed when the “intrinsic” immunity of cells is impaired and does not depend on interferon cascades. Interestingly, this mechanism has also been found in stem cells.
Examples of Other Stressors: Sleep Deprivation
Another type of stressor, sleep deprivation, has a similar effect on microglia. Short-term (6 hours) acute sleep deprivation leads to increased cytokine release and increased ramification of microglial cells in the brains of animals. The latter is a compensatory mechanism that helps form more functional connections with the microenvironment, synapses, and neighboring cells. During the recovery period after sleep deprivation, microglia are involved in the restoration of nervous tissue, regulation of synaptic homeostasis, and memory.
With prolonged chronic sleep deprivation (up to 5 days in a row), microglia cells take on an amoeboid, deramified or adendritic form. This, most likely, reflects a different type of behavior that can be found in severe CNS lesions, rather than the “homeostatic” or “stabilizing” responses of the brain to this type of stress.
At the genomic level, sleep deprivation leads to changes in genes associated with the modulation of neuronal activity, synaptic plasticity, transcription, and translation. For example, in mice without microglia, sleep deprivation change the morphological characteristics of neurons – a decrease in the density of dendritic spines. At the same time, in healthy animals, their density, on the contrary, increases.
Thus, it can be assumed that with a lack of sleep, microglia has a positive effect on the surrounding cells – it participates in stabilizing the physiological microenvironment and the functional state of neurons, and does not initiate inflammatory or other pathological immune processes. Adaptation is a complex, multifaceted process that affects all levels of a living organism, from the brain to the cell and vice versa.

Conclusion
So, what causes stress in the brain? The brain is the first to perceive a signal of danger and launches a cascade of psychophysiological, neurochemical, and molecular-genetic reactions. Through intermediaries – the immune and endocrine systems – the signal is transmitted and detected by microglial cells.
According to the mechanism of positive or negative feedback, they determine what the further systemic response to stress will be. All this again raises fundamental questions about the extent to which the psychophysiological characteristics of the body are determined by subtle molecular-genetic processes, and to what extent by external influences.